Results
#1. A patient is diagnosed with long QT syndrome and has been commenced on beta-blockers with no symptoms and a QTc of 470 ms. No genetic testing has been performed. She has a 7-year-old daughter and asks about the risks for her child. What is it appropriate to tell her?
An increasing number of genes have been identified for the long QT syndrome
but approximately 80% of patients have a mutation of one of three genes (LQT–3).
It is always best to perform genetic tests on the subject who has the clearest case of the
condition. In this case, this is the patient herself. If a culprit gene can be found, the process
of screening family members becomes much simpler.
#2. . A 61-year-old with a history of a myocardial infarction 2 years ago with a known ejection fraction of 25% presents to A&E with a 2 hour history of mild palpitations. He is otherwise fit and well. His ECG monitoring shows a regular broad complex tachycardia at a rate of 170 bpm which self-terminated before a 12-lead ECG was performed. His U&Es are normal. The patient’s blood pressure was 130/90 mmHg during the tachycardia and he was not unduly distressed. He is transferred to CCU where a 12-lead ECG shows LBBB with a QRS duration of 100 ms.
This man is very likely to have sustained ventricular tachycardia (VT) given his history
of ischaemic heart disease, impaired ejection fraction, and broad complex tachycardia.
The fact that he has tolerated it well is not an indication that it is an SVT, although this is
possibleS Therefore an ICD is indicated by NICE criteria as he has an EF <35%, sustained
VT, ischaemic aetiology, and NYHA class III or lessS It should be noted that this is a secondary prevention indication despite the fact the patient does not appear to have been
compromised by his VTS NICE recommends a VT stimulation study for non-sustained VT
(NSVT) and EF <35%, but the patient already meets criteria for an ICD and therefore
this would be a redundant investigationS Flecainide is contraindicated in patients with established IHD or structural heart diseaseS
#3. A patient with previous myocardial infarction, an ejection fraction of 25%, and a QRS duration of 140 ms, but no history of cardiac arrest, is seen in clinic and an ICD is recommended. She is concerned about driving. What is it appropriate to tell her?
The ICD would be a primary prevention device and therefore the patient needs to stop driving for 1month (compared with 6 months for a secondary prevention device). However, if she has an appropriate shock it is then treated in the same way as a device implanted for secondary prevention and requires 6 months off driving
#4. Which one of the following features is least suggestive that a broad complex tachycardia is ventricular in origin (VT)?
P waves walking through the tachycardia and capture beats are evidence of independent P-wave activity and ‘prove’ that the rhythm is VTS If the QRS is broad in sinus rhythm, it indicates preRexisting conduction tissue disease which will not shorten if the tachycardia is an SVTS Therefore shortening of the QRS proves that the rhythm is VT, probably originating from the septum to give a relatively narrow QRSS Negative concordance shows that the rhythm is originating from the apex of the heart and is therefore VTS The rsR’ pattern is seen in typical RBBB and is suggestive of aberrancy rather than VT, although this is not diagnosticS
#5. Which one of these drugs does not prolong the QT interval?

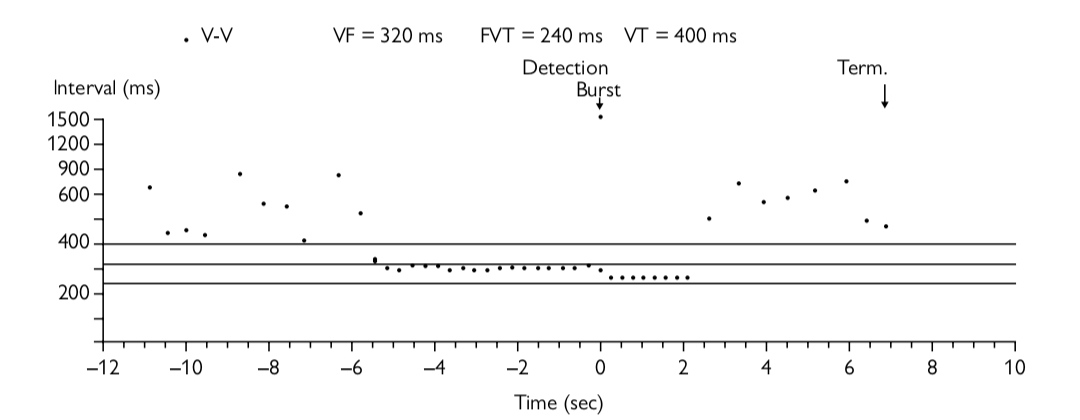
#6. What does the the box plot in Figure show?
This is a singleRchamber ICD and therefore there is no information from the atrium. At the beginning of the trace the RR intervals are irregular and relatively long (none are less than 100 ms). This is due to underlying AF.There is then a sudden increase to a regular tachycardia with a cycle length of 300 ms (rate 200 bpm) which is entirely consistent with VT. There are 18 of these beats before the device appropriately detects VT, marked with the word detection appearing at time point 0. The giveaway that ATP is delivered is the word ‘Burst’ being documented, but it can also be seen that 8 beats occur at a slightly shorter RR interval than the VT before the successful termination of the VT and a return to AF with a slower irregular RR intervalS These 8 beats are the ATP being delivered. It is important to scrutinize all the information on the programmer printouts carefully as each manufacturer gives the information in a different format.
#7. A 65-year-old diabetic man with a previous history of myocardial infarction 3 years ago (no intervention required) is found to have atrial fibrillation. His LVEF is 55% and he has no cardiovascular symptoms. What would you advise him with regard to the best thromboprophylaxis?
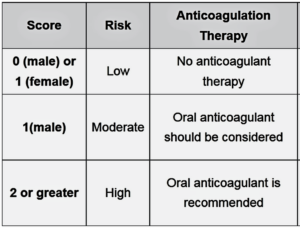
This man has a CHADS2 score of 1 (one point for diabetes) and therefore could be offered warfarin or aspirin thromboprophylaxis according to this risk stratification system.
However, if the newer CHA2DS2RVASc system is used, he has a score of 3 ( one point for each of DM, age 65–74, and previous MI) and should be offered oral anticoagulation (warfarin or newer agents). A CHA2DS2RVASc score of zero is truly low risk and could be managed with no thromboprophylaxis at all or aspirin Mno thromboprophylaxis preferable). A CHA2DS2RVASc score of 1 could be managed with aspirin or oral anticoagulation ( the latter is preferable). A score ≥2 should be managed with oral anticoagulation. In summary oral anticoagulation is preferred to aspirin in AF patients with one or more stroke risk factors based on the CHA2DS2RVASc score. I 

 n the absence of recent ACS or coronary artery stenting, there is no good evidence for either warfarin or antiplatelet drugs.
n the absence of recent ACS or coronary artery stenting, there is no good evidence for either warfarin or antiplatelet drugs.
#8. A 25-year-old man presents to the ED with a broad complex tachycardia that is irregularly irregular. The patient is haemodynamically uncompromised. An anaesthetist is not available to assist with immediate DC cardioversion. What is the best initial treatment option?
This man may have an accessory pathway with rapidly conducted AFS Adenosine, Digoxin, verapamil, and betaRblockers should all be avoided as they prolong the AV node refractory period and thus may increase conduction down an accessory pathway. This increases the risk of rapidly conducted AF becoming VF. Intravenous class I antiarrhythmic drugs (eg. procainamide, flecainide, propafenone) can be used as well as amiodarone, but DC cardioversion is the treatment of choice if there is haemodynamic compromise or rapidly conducted AF down an accessory pathway.
#9. A 60-year-old man attends clinic because of hypertension. His BP in clinic is 70/90 mmHg and his echocardiogram shows mild LVH and mild LA dilatation. He is not diabetic and has no other medical history of note. Which one of the following medications is most effective in preventing AF?
ACE inhibitors and ARBs have antifibrillatory and antifibrotic properties. A meta analysis has shown that ACE inhibitors and angiotensin receptor blockers (ARBs) reduce the relative risk of incident AF by 25%. The LIFE study, in particular, showed a 33% reduction in new onset AF in patients with LVH treated with losartan compared with those treated with atenolol.
#10. A 62-year-old woman attends clinic following an ED attendance 6 weeks previously with a one-week history of palpitations. She was diagnosed with AF at the time and commenced on aspirin and a beta-blocker. Her echocardiogram showed no significant abnormalities and her ECG in clinic today confirms atrial fibrillation with a ventricular rate of 70 bpm. She continues to get occasional palpitations and would like to be considered for cardioversion. What do you advise?
Patients should be anticoagulated with a therapeutic INR M>2) for at least 3 weeks prior to cardioversion. Anticoagulation should be continued for at least 4 weeks
- post cardioversion as ‘atrial stunning’ may occur. Anticoagulation is required prior to both chemical and electrical cardioverison. If a patient has not had oral anticoagulation for at least 3 weeks, it is reasonable to perform DC cardioversion if a TOE rules out left atrial thrombus. However, LMWH should be commenced prior to a TOE guided cardioversion and continued post cardioversion until the target INR is reached with oral anticoagulation.